Vitamin D is a big deal. Recent studies have shown that patients with low Vitamin D levels are more likely to die from Covid-19 than their Vitamin D-rich counterparts,(1) and deficiency in the vitamin has been linked to seven of the ten leading causes of death in the U.S.(2) These facts alone have been enough incentive for many people to start supplementing the vitamin. A common question from my patients is: how much Vitamin D should I take? This is a simple question, but there are a lot of assumptions built in. Before you order that case of Vitamin D for you and your family, let’s back up and look a little more at the data.
First, why I’m interested in Vitamin D: I’m a parathyroid surgeon, and the vitamin is something I track closely in my patients. For background, the parathyroid glands are tiny endocrine organs in your neck that regulate blood calcium levels. They do this partly through the activation of Vitamin D, which helps the intestines absorb calcium. Without Vitamin D, you will have difficulty getting enough calcium, even if you are taking calcium supplements. Your bones need calcium, so a severe deficiency in Vitamin D leads to bone deformities in children (rickets) and bone loss in adults (osteomalacia).
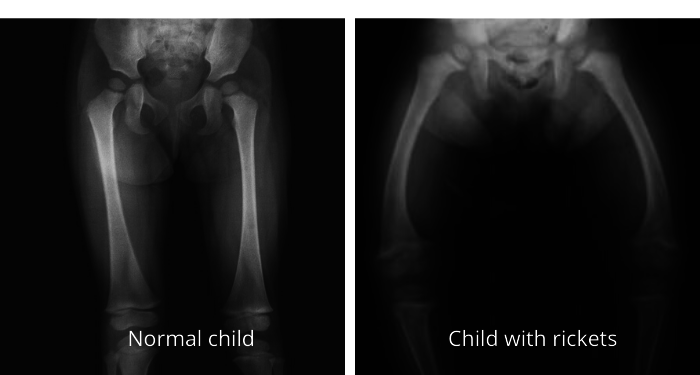
Normal child femurs compared to femurs of a child with rickets. Rickets is caused by a severe Vitamin D deficiency while bones are growing. This condition is now very rare in the U.S. due to the fortification of almost all milk with Vitamin D.*
The relationship between parathyroid hormone, calcium, and Vitamin D is complex and fascinating (at least to a parathyroid surgeon), but the vitamin appears to do much more than just influence calcium. We’re still figuring out all that it does, but we have some circumstantial evidence about its roles. Low Vitamin D levels are linked to a variety of illnesses including cancers, hypertension, diabetes, obesity, heart failure, stroke, dementia, autoimmune disease, and respiratory tract infections (including Covid-19). A simple search of the medical literature on PubMed produces page after page of articles on the harms of Vitamin D deficiency.
Most studies follow this pattern: Two sets of people are evaluated. One set has a certain disease (diabetes, for example). The other set does not have the disease. Vitamin D levels are measured in both groups. Vitamin D deficiency is found to be much more common in the group of diseased individuals.
Using this study method, Vitamin D deficiency is correlated with many diseases. But correlation does not equal causation. The fact that two things are related does not imply that one caused the other. With regard to the vitamin and diabetes, it could be that diabetes causes low Vitamin D. Or it may be that some other health condition causes both low Vitamin D and diabetes. Obesity, for example, is a known risk factor for diabetes, and people who are obese also tend to have low Vitamin D levels, due mostly to the dilution of the fat-soluble vitamin in the larger mass of adipose tissue. The close association between Vitamin D and diabetes could be due simply to the association they both share with obesity.
Here is another example: Early interest in respiratory infections and Vitamin D was due to research on hospitalized children. Young children who were hospitalized with respiratory infections were found to have much higher rates of rickets than children hospitalized for other causes.(3) Rickets, of course, is caused by Vitamin D deficiency. If Vitamin D deficiency also causes immune dysfunction, we might come up with an explanation for how low Vitamin D in these children made them more susceptible to infection. But there are other explanations. Children with a serious vitamin deficiency are likely to be less healthy overall compared to non-deficient children. In addition, rickets can cause rib deformities, which are known to make it harder to cough and breathe deeply, leading to an increased risk of respiratory infections. Vitamin D itself is not necessary for explaining the infections in these children.
Most researchers understand that correlation does not equal causation. The classic example of this involves the correlation between ice cream and violent crime. As ice cream consumption rises, so does the rate of violent crime. The association is strong, and puzzling, until you remember that more ice cream is sold during warmer months, which is also when violent crime rates rise. Ice cream has no causative connection to crime.

Children about to embark on a life of crime?
But the temptation to equate correlation and causation is strong. Many articles showing a correlation with Vitamin D will add an untested but completely plausible physiological explanation for how low vitamin levels could lead to the disease. Armed with a solid correlation and a reasonable argument for causation, they may feel justified in concluding that the evidence for causation is strong. And once you have made that leap, you are almost obligated in recommending Vitamin D supplementation for anyone affected by or concerned about your disease of interest.
Assuming that the correlations between Vitamin D and various illnesses are accurate, the argument for supplementation then depends on the plausibility of the physiologic mechanism. The numerous conditions associated with the deficiency involve disparate organs and body systems. To understand how one vitamin could be involved in so much, and whether we can explain a disease state by the vitamin's deficiency, it helps to know the basics of what Vitamin D does on a molecular level.
Vitamin D is a hormone that binds to the Vitamin D Receptor, a protein made by cells throughout your body. The vitamin acts like a key, while the receptor is a lock. A key and lock are pointless individually, but useful together. Vitamin D and its receptor are inactive until they combine, and then they interact with DNA to produce certain actions within the cell. Based on what we already know, it is easy to understand why the intestines, parathyroids, and bones make Vitamin D Receptors – these organs are all involved in regulating calcium levels, and we know Vitamin D regulates calcium metabolism. But those are not the only organs that have the receptors. We find these receptors all over the place, in the kidneys, lungs, pancreas, uterus, and blood cells involved in immune function, just to name a few.(4,5)
Our bodies like to conserve resources, so if an organ or cell uses energy and resources to make these receptors, we can assume that they use them. This is the first solid piece of evidence that Vitamin D is involved in many processes throughout multiple organs. The next goal is to figure out how the organs use Vitamin D. There are various ways to do this. One clever method involves the use of mutant mice called “knockout mice” that have been genetically modified to inactivate a specific gene. In this case, the gene for the Vitamin D Receptor is inactivated, to produce "VDR null" mice. Studies in these animals provide important clues about Vitamin D, since without the lock, or receptor, the key is useless. As expected, these knockout mice have problems with calcium absorption, and the most notable effect is stunted bone growth.(6) This can be mitigated by giving the mice lots of calcium, which makes sense, since it is possible but harder for calcium to be absorbed without Vitamin D.
Knockout mice are mice that have been genetically modified to inactivate a specific gene. VDR null mice are knockout mice that do not make Vitamin D Receptors. (The mouse in the photo is just a random mouse. We don't actually grow them in petri dishes.)
But we already knew about Vitamin D and calcium. What about those other effects? VDR null mice should be helpful in explaining Vitamin D’s other roles, and we do see some revealing changes: these mutant mice on average have higher blood pressure than normal mice, and mice lacking the receptor specifically on the heart have decreased cardiac function. Certain immune cells also seem to also be impaired in the mutant mice.
Following this out a few steps, we could come up with a logical explanation for how Vitamin D helps the immune system, and thus deficiency would lead to impaired immune function, which then lead to increased susceptibility to infections. It sounds reasonable. But there are a few assumptions we are making: 1. We assume that Vitamin D deficiency is similar to a complete absence of the receptor. This is questionable, since even people with severe Vitamin D deficiencies still have some amount of Vitamin D. 2. We also assume that the receptor works exactly the same in mice as it does in humans. Mice and humans are relatively close on the evolutionary tree (when compared to, say, shiitake mushrooms), so this could be true, but maybe not.
Maybe we need to go back to humans. Interestingly, there is a very rare condition in humans characterized by ineffective Vitamin D Receptors due to a genetic mutation, similar to the VDR null mice.(7) Like the mice, these individuals will develop severely abnormal bone growth if untreated. Thinking logically and using what we know about the receptor in mice, we might expect that these individuals who cannot process Vitamin D effectively would have immune dysfunction, and perhaps cardiac issues. So far, we have not seen this. They do not appear to have an increased risk of cancer, respiratory infections, diabetes, or any of the other conditions found to be associated with Vitamin D deficiency. This genetic defect is extremely rare, though, and we have not yet been able to study these patients over a lifetime, so we may have more to learn.
Studying the Vitamin D Receptor in living bodies is not the only way to assess Vitamin D’s actions. We can also study Vitamin D in a lab, using living cells in a test tube or culture dish. Much of our evidence for a link between Vitamin D and immunity comes from these in vitro studies. Vitamin D Receptors are common in many types of immune cells, and Vitamin D exposure leads to a well-documented cascade of changes within those.(8) These studies provide the best evidence for Vitamin D’s role in immunity, which could explain its roles in autoimmune disease and infections.
In vitro studies are necessarily contrived and artificial, which is great for isolating and quantifying the effect of one stimulus, but which is not always applicable to living cells in vivo. Within a living organism, cells are not restricted to interacting with just one molecule at a time. There are many interactions going on simultaneously, diluting or hiding the effects of Vitamin D. These other interactions could potentially inhibit or enhance the vitamin’s effects, but it will be much more difficult to quantify that. Still, in vitro studies of Vitamin D and various cell cultures provide strong evidence that Vitamin D is at least capable of inducing major changes in the actions of certain cells.
Unfortunately, we do not have a full unified explanation for how Vitamin D deficiency could lead to the list of diseases that are associated with it. We know the correlations are there, and we can show that the Vitamin D molecule has an effect on multiple cells and organs. But this is clearly not as straightforward as the role of Vitamin D in calcium metabolism and bone health.
There is more to the story, of course, which will continue in part 2. And eventually we will get to those recommended dosages.
*Rickets image by ,Michael L. Richardson, M.D. at English Wikipedia. / CC BY-SA (https://creativecommons.org/licenses/by-sa/1.0).
From us to your inbox weekly.